Cervical Screening (Smear)
Cervical Screening
Click here to view:
Your guide to NHS Cervical Screening
- Why the NHS offers cervical screening
- Who we invite for cervical screening
- Cervical cancer and HPV
- How cervical screening works
- At your appointment
- Practical hints and support
- Cervical screening results
- Possible risks of cervical screening
- Cervical cancer symptoms
- Who is more likely to get cervical cancer
- Cervical cancer and the HPV vaccine
- Clinical trials
- More information and support
Changes to the Cervical Screening Programme - 1st July 2025
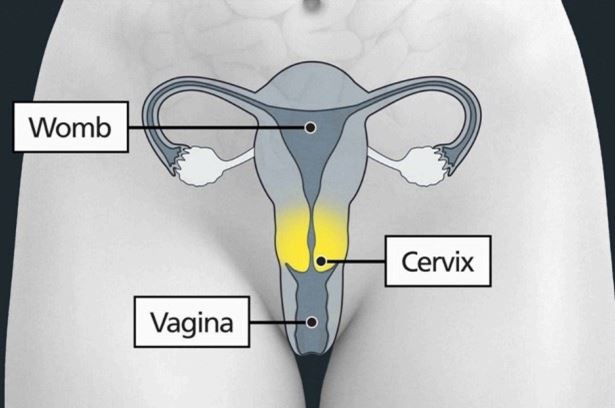
The NHS Cervical Screening Programme saves thousands of lives every year by detecting abnormal cells in the cervix that could develop into cancer, if left untreated.
How often people need to have cervical screening is changing in England from 1st July 2025. Improvements in HPV testing enables the NHS to now offer a more personalised approach to preventing cervical cancer, which means those identified as lower risk won’t need to be screened as frequently, and those at higher risk will continue to be monitored more regularly.
The Human Papillomavirus (HPV) causes nearly all cervical cancers. Since December 2019 all cervical screening samples taken in England have been tested for high-risk HPV. It is a more sensitive and accurate test than the previous method and is the best way to find out who is at higher risk of developing the cell changes that over time could lead to cervical cancer.
At the moment, in England, women and people with a cervix aged 25-49 years are routinely invited for screening every 3 years. Now we have this better test for HPV, the UK National Screening Committee (UKNSC) has recommended that those testing negative, and with no recent history of HPV, won’t need to come for a cervical screening quite so often – every 5 years instead of every 3. If your cervical screening shows you have HPV, you may be invited for more frequent screenings to check HPV has cleared and if not, if any cell changes have developed.
This change is strongly backed by robust scientific evidence. Studies have shown that if a person tests negative for HPV they are extremely unlikely to go on to develop cervical cancer within the next 10 years. Research published by King’s College London showed that 5-yearly screening is as safe as 3-yearly; the same number of cancers will be prevented and less frequent cervical screening tests are needed.
This move brings England into line with Scotland and Wales who have introduced this change, and with women aged 50 – 64 who are already invited every 5 years.
The positive impact of the HPV vaccination is also starting to be seen, with studies in England showing that the HPV vaccine stops 90% of cervical cancer cases. The latest HPV vaccine type introduced in the UK in 2021 is predicted to further reduce cases of women’s cancer and HPV attributable deaths by 16% and 9%, compared to the previous vaccine type.
Even if you've had the HPV vaccination, it's important that you attend your cervical screening. Cervical screening saves lives – so make sure you come forward for your screening when you’re invited, even if it was weeks, months or years ago. If you think you are due but have not yet had an invitation, speak to your GP practice.
Digital correspondence
The NHS Cervical Screening Programme has introduced digital invitations and reminders via the NHS App. Eligible people will now receive screening invitations and reminders through the NHS App when they're due. For those where a digital invitation isn’t possible, a letter will be posted as a backup. All invitations will guide participants to book appointments in the usual way. We would encourage everyone to download the NHS App: www.nhs.uk/nhs-app/ and enable notifications.
This digital transformation supports the NHS commitment to put patients in control of their own healthcare, making it easier to manage appointments and health needs.
Page created: 10 September 2021